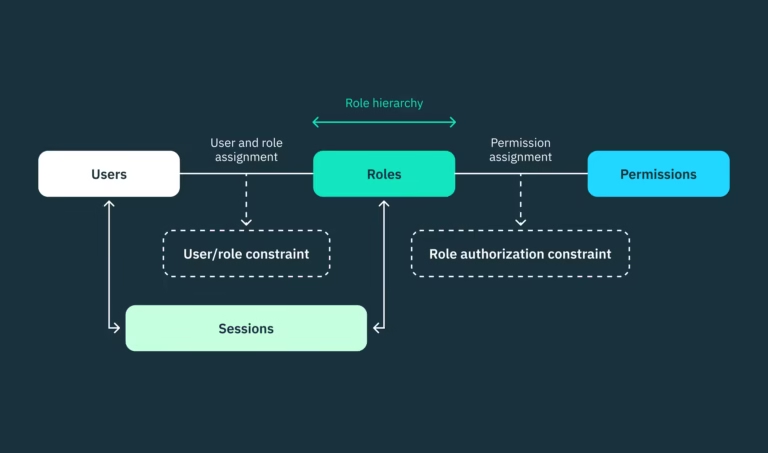
Understanding the Gut-Brain Axis
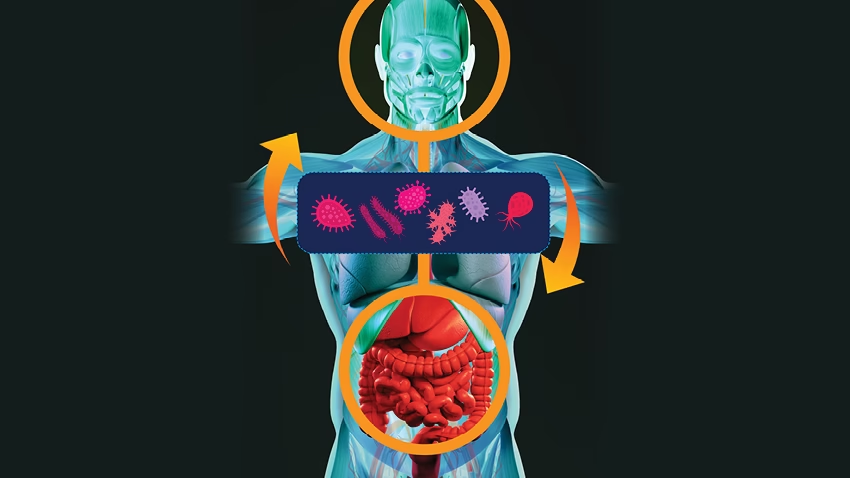
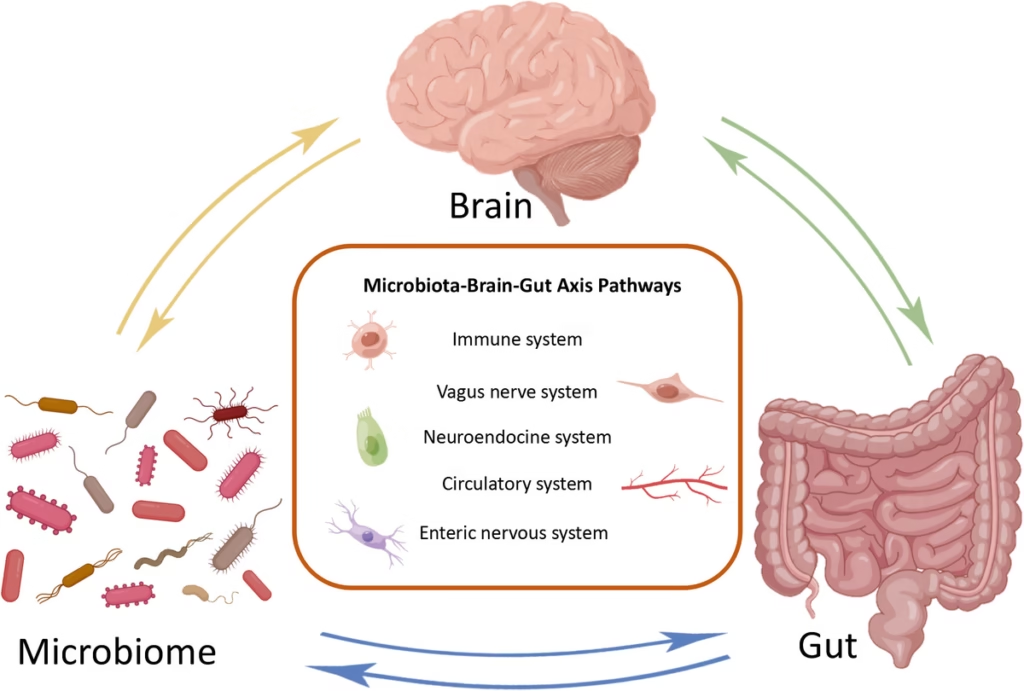
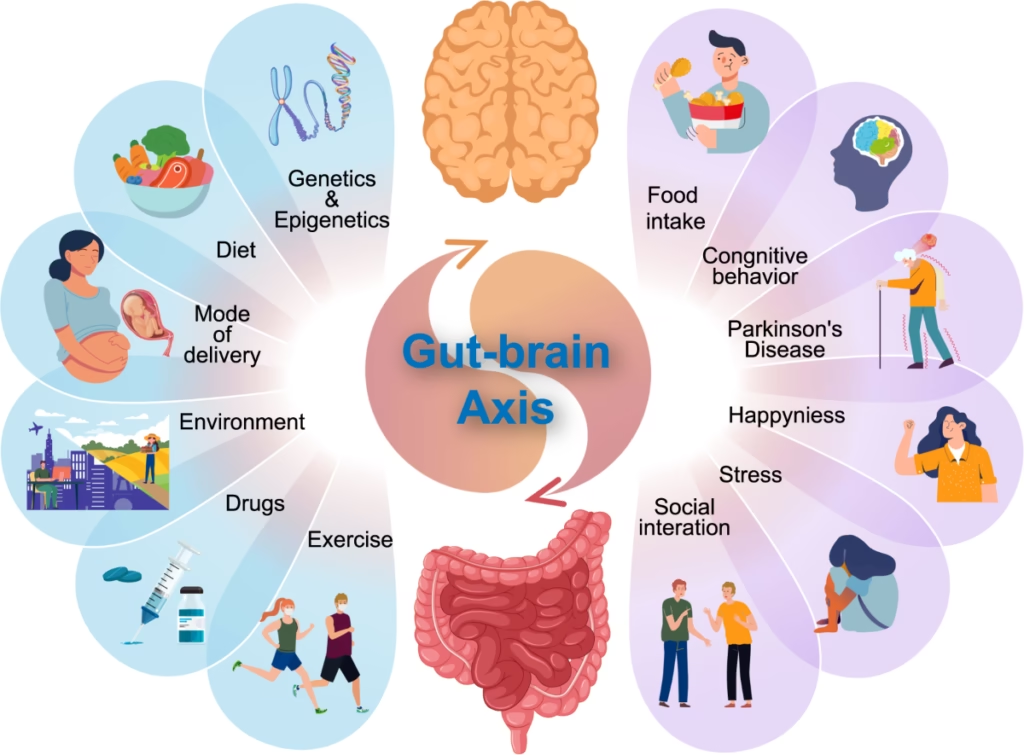
The gut-brain axis refers to the complex communication network that links the gastrointestinal system with the brain, highlighting the significant interplay between these two critical systems. This bi-directional communication involves multiple pathways, including neural, hormonal, and immunological routes. One of the key components of this interaction is the vagus nerve, which serves as a primary conduit for signals traveling between the gut and the brain. It plays an essential role in relaying sensory information from the digestive tract to the central nervous system, influencing emotional and cognitive processes.
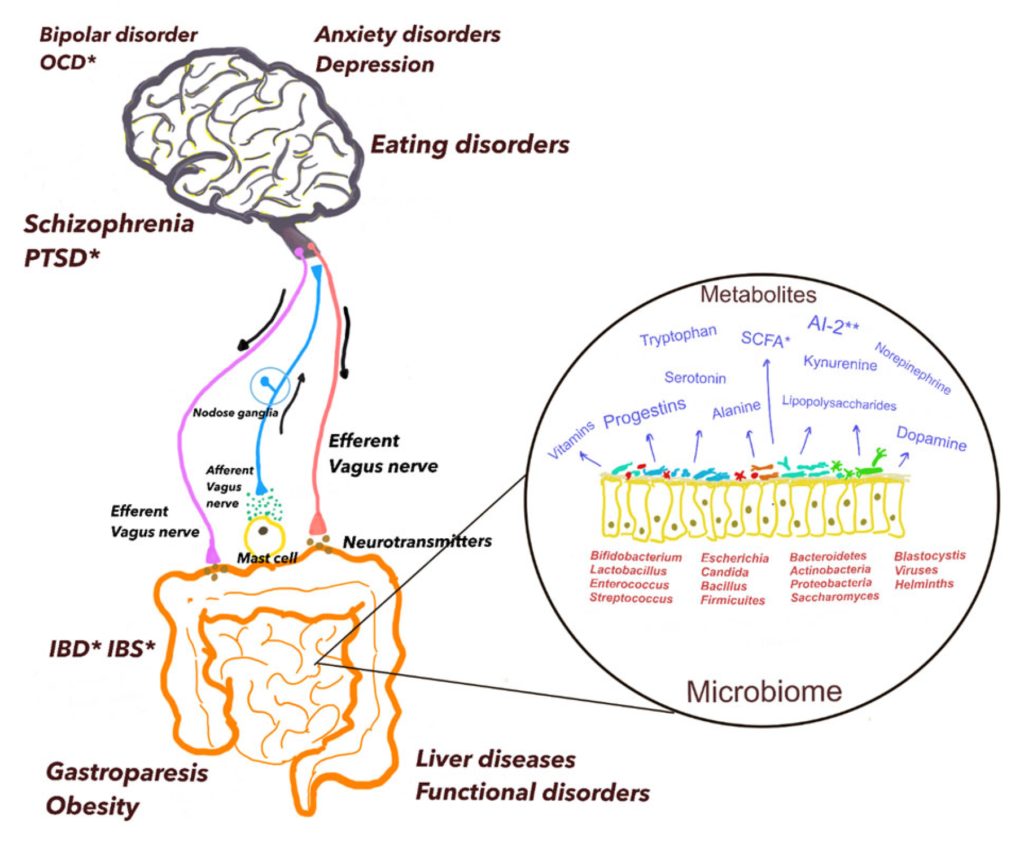
Moreover, the gut microbiome, consisting of trillions of microorganisms, can also affect brain function and mood. These microorganisms produce various metabolites, including short-chain fatty acids and neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), which can influence mood regulation. In fact, about 90% of serotonin, a key mood-regulating neurotransmitter, is produced in the gut, underscoring the microbiome’s potential impact on mental well-being.
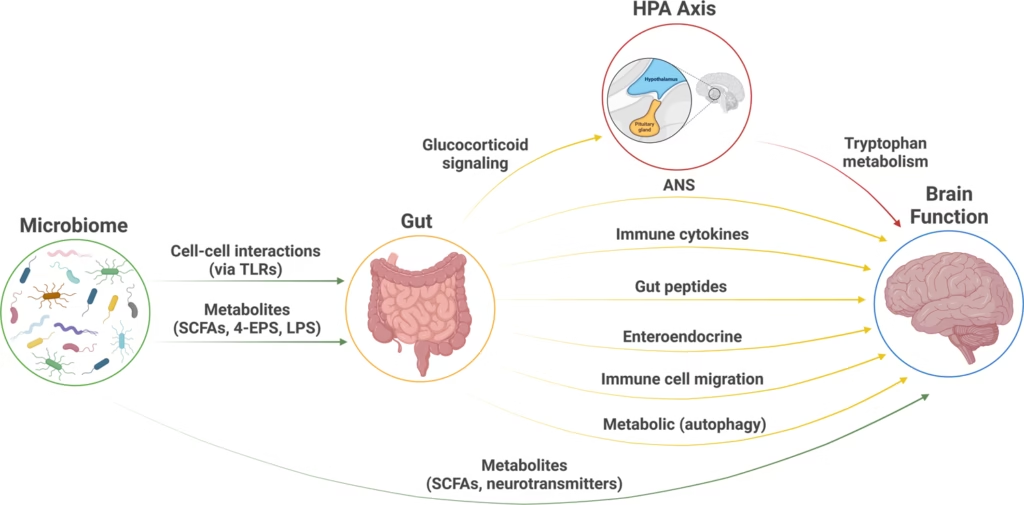
The endocrine system further contributes to the gut-brain axis by releasing hormones that are affected by gut health. The microbial community can modulate the release of stress hormones and other biochemical signals, affecting how we respond to stress and anxiety. This interaction suggests that disruptions in gut microbial balance might lead to a cascade of hormonal changes that adversely impact mood and mental health.
Understanding the gut-brain axis is essential not only for comprehending how gastrointestinal health relates to emotional health but also for exploring therapeutic avenues that leverage this connection. As research in this area progresses, it points to the gut microbiome as a promising factor in managing various mood disorders and highlights the importance of maintaining a healthy digestive system to support mental wellness.
The Science of the Gut-Brain Axis
The gut-brain axis (GBA) is a complex network linking the central nervous system (CNS) and the enteric nervous system (ENS), often referred to as the “second brain.” This communication occurs through neural pathways, chemical signals, and hormonal exchanges. Key players in this system include:
The Microbiome: The diverse microbial community in the gut plays a pivotal role in modulating these interactions
The Vagus Nerve: A major communication highway connecting the gut and brain. It transmits signals both ways, influencing mood, digestion, and immune responses.
Neurotransmitters: The gut produces neurotransmitters like serotonin and dopamine, which are critical for mood regulation.
The Role of the Microbiome
The human microbiome is a complex ecosystem consisting of trillions of microorganisms, including bacteria, viruses, fungi, and protozoa. This diverse community inhabits various body sites, predominantly the gastrointestinal tract, where it plays a crucial role in maintaining health. The composition and diversity of the microbiome can significantly influence numerous physiological functions, including digestion, metabolism, and immune responses. Importantly, the gut microbiome has garnered considerable interest for its intricate relationship with mental health and emotional well-being.
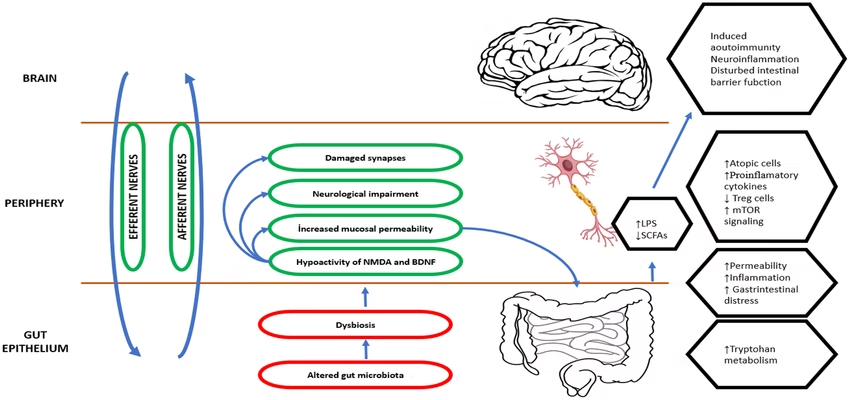
The microorganisms present in the gut assist in breaking down food, synthesizing essential nutrients, and filtering harmful substances. Various bacterial species, such as Firmicutes and Bacteroidetes, are vital for effective nutrient absorption and energy extraction from dietary components. Furthermore, the microbiome contributes to the development and regulation of the immune system, thereby helping defend against pathogenic microorganisms and reducing inflammation. An imbalance within this microbial community, often referred to as dysbiosis, has been linked to several health issues, including gastrointestinal disorders, obesity, and autoimmune diseases. Additionally, emerging research indicates that dysbiosis might also impact mental health.
The gut-brain axis is a bidirectional communication network connecting the gastrointestinal tract and the central nervous system. This intricate relationship suggests that the gut microbiome may influence mood and behavior through various mechanisms, such as the production of neurotransmitters, modulation of the immune system, and effects on the enteroendocrine system. For instance, certain gut bacteria can produce serotonin, a neurotransmitter essential for regulating mood, thus demonstrating the profound impact of the microbiome on mental health. Cultivating a diverse and balanced microbiome may therefore be an important strategy for enhancing overall well-being, including emotional and psychological resilience.
Microbiome and Neurotransmitters
The human microbiome, comprising trillions of microorganisms, has gained recognition as a vital player in influencing various physiological processes, particularly the production and regulation of neurotransmitters. Among these chemical messengers, serotonin and dopamine are of paramount importance due to their profound implications for mood and emotional well-being. Research indicates that the gut microbiota significantly impacts the synthesis of these neurotransmitters, thereby creating a crucial link between intestinal health and mental health.
Empirical studies have demonstrated that certain gut bacteria are capable of producing neuroactive compounds. For example, certain strains of Lactobacillus and Bifidobacterium have been shown to produce serotonin precursors, which can subsequently influence mood regulation. Serotonin, often referred to as the ‘feel-good’ neurotransmitter, is primarily synthesized in the gut, where approximately 90% of it is found. An imbalance in gut microbiota can disrupt serotonin production, potentially leading to mood disorders such as anxiety and depression.
Dopamine, another critical neurotransmitter involved in reward and pleasure pathways, is similarly influenced by the microbiome. Gut bacteria can impact dopamine levels directly by producing metabolites that either stimulate or inhibit dopamine receptors or indirectly by modulating systemic inflammation and gut permeability, which can, in turn, affect neurotransmitter signaling. These findings underscore the importance of maintaining a healthy gut microbiome to support balanced neurotransmitter levels.
Several studies have explored the relationship between alterations in gut microbiota composition and neuropsychiatric conditions. For instance, evidence suggests that individuals with depression or anxiety often exhibit dysbiosis, an imbalance of gut bacteria. This dysbiosis can impair the production of key neurotransmitters, thereby exacerbating mood disturbances and illustrating the complex interplay between the microbiome and mental health. The ongoing research continues to unravel these mechanisms, indicating that a robust microbiome could play a pivotal role in fostering better emotional health.
How the Microbiome Shapes Mood
Gut-Derived Short-Chain Fatty Acids (SCFAs)
Beneficial bacteria produce SCFAs like butyrate, which support the integrity of the gut lining and reduce systemic inflammation. Healthy SCFA production is associated with improved mental clarity and reduced anxiety.
Neurotransmitter Production
The gut is responsible for producing approximately 90% of the body’s serotonin, a key mood-regulating chemical. Certain gut bacteria, such as Lactobacillus and Bifidobacterium, are involved in the synthesis of serotonin precursors. An imbalance in these microbes, known as dysbiosis, can disrupt serotonin levels, potentially leading to anxiety or depression.
Stress Response Regulation
The microbiome influences the hypothalamic-pituitary-adrenal (HPA) axis, which governs the body’s stress response. Research shows that a healthy gut can dampen the stress response, while dysbiosis may exacerbate it.
Inflammation and Mood
Chronic gut inflammation, often caused by an unhealthy diet or infection, releases pro-inflammatory cytokines. These molecules can cross the blood-brain barrier and trigger neuroinflammation, which is linked to depression and cognitive decline.
Impact of Diet on the Microbiome
The microbiome is increasingly recognized for its central role in maintaining not only gut health but also the overall well-being of an individual, including their mood. Diet plays a crucial role in shaping the composition and diversity of the gut microbiota. Certain dietary choices can significantly influence the microbial ecosystem within the gastrointestinal tract, affecting how the microbiome interacts with the brain.
One of the most vital components of a diet that supports a healthy microbiome is dietary fiber. High-fiber foods, such as fruits, vegetables, whole grains, legumes, and nuts, serve as prebiotics. These substances are not digestible by the human body but can be fermented by beneficial gut bacteria, which thrive on such nutrients. Increasing fiber intake encourages the growth of a diverse community of microbes. This diversity is associated with various health benefits, including improved mood and reduced risk of mental health disorders.
Probiotic-rich foods also play a significant role in enhancing microbiome health. Fermented products such as yogurt, kefir, sauerkraut, and kimchi contain live beneficial bacteria that can help restore and maintain a balanced gut microbiome. Consuming these foods regularly can aid in promoting microbial diversity, which has been linked to improved emotional health and a reduction in symptoms of anxiety and depression.
Moreover, dietary patterns encompassing a Mediterranean diet, which emphasizes plant-based foods, healthy fats, and lean proteins, have shown promise in fostering a robust microbiome. Such diets are not only rich in essential nutrients but also contribute to the growth of beneficial bacteria. In essence, a thoughtful approach to dietary choices allows individuals to positively influence their microbiome, thereby enhancing mood and emotional health.
The Role of Diet in the Gut-Brain Connection
Reducing Processed Foods
Processed foods and high sugar intake disrupt the microbiome, leading to dysbiosis and mood swings.
Fiber-Rich Foods
High-fiber diets promote the growth of beneficial bacteria that produce SCFAs, aiding mood stabilization.
Probiotics and Prebiotics
Fermented foods like yogurt, kimchi, and kefir introduce beneficial bacteria, while prebiotics (e.g., bananas, garlic, and asparagus) feed existing microbes.
Polyphenol-Rich Foods
Foods like berries, green tea, and dark chocolate contain polyphenols, which act as antioxidants and support gut health.
Omega-3 Fatty Acids
Found in fish and flaxseeds, omega-3s reduce inflammation and enhance neurotransmitter function.
Psychobiotics: The Connection between Probiotics and Mental Health
Psychobiotics represent a fascinating intersection between gut health and mental well-being. These specific strains of probiotics are believed to have beneficial effects on mood and emotional health, potentially alleviating symptoms associated with anxiety and depression. The gut microbiome, consisting of trillions of microorganisms, communicates with the brain through various pathways, influencing both psychological and physiological processes. This bidirectional communication, often referred to as the gut-brain axis, has sparked significant interest within the scientific community, leading to numerous studies exploring the impact of psychobiotics on mental health.
Research has shown that certain strains of probiotics, particularly Lactobacillus and Bifidobacterium, can have a positive impact on psychological well-being. For instance, a study published in 2016 found that individuals who consumed probiotics exhibited reduced levels of anxiety and lower perceived stress levels compared to a control group. These findings suggest that by modulating the gut microbiome, psychobiotics can contribute to improved mental health outcomes.
Moreover, psychobiotics may help in the treatment of more severe mental health disorders. Some clinical trials have demonstrated that these probiotics can enhance mood and even serve as adjuncts to traditional anxiety and depression treatments. For example, participants in a randomized controlled trial reported significant improvements in depressive symptoms after taking psychobiotic supplements for eight weeks. This suggests that integrating psychobiotics into daily routines may provide a novel approach for individuals seeking complementary strategies for managing their mental health.
As consumer interest in gut health continues to rise, the potential of psychobiotics is becoming increasingly recognized. Products that contain these beneficial microorganisms are now widely available, ranging from dietary supplements to functional foods. Nevertheless, while the research is promising, further studies are warranted to fully understand the mechanisms behind psychobiotics and their effects on mental health. Ultimately, the connection between probiotics and emotional well-being could pave the way for innovative mental health interventions in the future.
Mental Health Disorders Linked to the Gut-Brain Axis
Parkinson’s Disease
Emerging evidence indicates that gut dysfunction may precede the onset of Parkinson’s, highlighting the role of the microbiome in neurodegenerative diseases.
Depression
Studies have shown that individuals with depression often have reduced microbial diversity. Probiotic supplementation has demonstrated potential in alleviating depressive symptoms.
Anxiety
A dysregulated gut can amplify the body’s stress response. Gut-focused therapies, such as probiotics and dietary changes, have shown promise in reducing anxiety.
Autism Spectrum Disorder (ASD)
Research suggests that children with ASD have distinct gut microbiota profiles, and gut-targeted interventions are being explored as part of treatment plans.
Stress, Gut Health, and the Microbiome
The intricate relationship between stress, gut health, and the microbiome has garnered substantial attention in recent years, illustrating how interconnected these aspects are in influencing overall well-being. The gut microbiome, composed of trillions of microorganisms, plays a significant role in regulating various bodily functions, including the immune system and metabolic processes. However, when an individual experiences stress, the microbiome’s delicate balance can be disrupted, leading to notable shifts in its composition and functionality.
Studies suggest that stress can significantly impact the diversity of gut bacteria, whereby beneficial microbes may decline, and harmful strains may proliferate. This alteration can result in increased intestinal permeability, often referred to as “leaky gut,” enabling toxins and pathogens to enter the bloodstream. Such disturbances not only compromise physical health but have also been linked to psychological conditions such as anxiety and depression. The chronic activation of the body’s stress response can further exacerbate these effects, creating a vicious cycle where mood disorders may lead to increased stress, perpetuating the cycle of gut dysfunction.
Furthermore, the relationship between stress and the microbiome underscores the importance of maintaining gut health to mitigate stress-related mood disorders. Probiotic and prebiotic interventions have shown promise in restoring microbial balance and enhancing resilience against stressors. As research continues to elucidate the gut-brain axis mechanisms, it becomes increasingly clear that fostering a healthy microbiome may offer a viable pathway to emotional well-being. Integrating stress-reduction techniques, such as mindfulness and regular physical activity, alongside dietary considerations can better support gut health, ultimately influencing mood and emotional stability in a positive manner.
Practical Strategies for a Healthy Gut and Mind
Maintaining a healthy gut is essential for optimal mental well-being. Several practical strategies can be implemented to promote a balanced microbiome, which in turn supports mood regulation and cognitive function. One of the most significant factors influencing gut health is diet. Incorporating a diverse range of fruits, vegetables, whole grains, and fermented foods into your daily meals can provide essential nutrients and probiotics that enhance gut flora. Foods like yogurt, kefir, sauerkraut, and kombucha are particularly beneficial, as they contain live cultures that may positively impact gut health.
Furthermore, adequate hydration plays a pivotal role in digestion and the overall function of the gut. Drinking enough water throughout the day can help in maintaining a healthy gut environment, which is vital for nutrient absorption and waste elimination. It is also essential to limit the intake of processed foods, artificial sweeteners, and excessive sugars, as they may negatively affect gut microbiota and contribute to mood disorders.
In addition to dietary modifications, regular physical activity has been shown to improve gut health and mental well-being. Engaging in moderate exercise, such as walking, cycling, or yoga, can stimulate the growth of beneficial bacteria in the gut and reduce symptoms of anxiety and depression. Aim for at least 150 minutes of moderate-intensity exercise weekly to reap the cognitive and physical benefits.
Stress management is another crucial component of maintaining a healthy gut-brain axis. Chronic stress can disrupt gut microbiota and exacerbate mental health issues. Incorporating mindfulness practices, such as meditation, deep breathing exercises, or spending time in nature, can help mitigate stress levels. Additionally, regular check-ups with healthcare providers are essential for early detection and management of gut-related issues that may impact mental health. By being proactive about gut and mental health, individuals can unlock the potential for a more balanced and fulfilling life.
- Incorporate Fermented Foods
Add yogurt, sauerkraut, and kombucha to your diet to boost beneficial bacteria. - Manage Stress
Practices like yoga, meditation, and mindfulness reduce stress, benefiting both the gut and brain. - Exercise Regularly
Physical activity promotes a diverse microbiome and releases endorphins that improve mood. - Sleep Hygiene
Poor sleep disrupts gut bacteria, while a healthy microbiome supports restful sleep. - Avoid Overuse of Antibiotics
Antibiotics can decimate beneficial bacteria. Use them judiciously and consider probiotics during treatment.

Emerging Therapies
Precision Medicine
Advances in microbiome research are paving the way for personalized gut-brain therapies tailored to individual needs.
Psychobiotics
These are probiotics specifically formulated to influence mental health. They hold promise for treating anxiety, depression, and other mood disorders.
Fecal Microbiota Transplantation (FMT)
FMT, though experimental, is being explored for its potential to restore microbiome balance in mood disorders.
Future Research Directions
The field of gut-brain communication and microbiome studies has witnessed significant advancements, yet numerous opportunities for exploration remain. Future research is poised to uncover the intricate mechanisms that link the gut microbiome and mood disorders, potentially transforming therapeutic approaches. A promising avenue of investigation involves the identification of specific microbial strains, metabolites, and their roles in influencing neurochemical pathways associated with mood regulation. Understanding these connections can enable the development of targeted probiotics or dietary interventions that may alleviate symptoms of anxiety and depression.
Another essential area for future research is the exploration of the gut microbiome’s response to environmental factors. The interplay of diet, lifestyle, stress, and microbial health can significantly impact mood. Investigating how these external variables affect the microbiome could lead to personalized therapeutic strategies that cater to individual needs. For instance, understanding how high-fiber diets or fermented foods influence gut bacteria may reveal new prevention approaches for mood disorders.
Moreover, advancements in genomic technologies offer the potential for more comprehensive mapping of the microbiome. As sequencing techniques become more sophisticated, researchers will be able to analyze complex microbial communities and their interactions within the gut. This information can facilitate the identification of biomarkers that may predict susceptibility to mood disorders, paving the way for early interventions.
Furthermore, the exploration of psychobiotics—live microorganisms that provide health benefits through an interaction with the gut-brain axis—remains an important frontier. Continued clinical trials examining the efficacy of these probiotics can provide vital insights into their therapeutic potential. It is crucial that future studies rigorously assess the safety and long-term effects of these interventions to establish their validity as treatment options.
In conclusion, the future of gut-brain research holds immense promise in reshaping our understanding of mood disorders and the microbiome. Continued advancements in this field may lead to innovative therapies that harness the power of our gut microbiota to improve mental health outcomes.
Conclusion
Throughout this blog post, we have explored the intricate relationship between the gut and the brain, shedding light on the concept of the gut-brain axis. This axis is a complex communication network that links our gastrointestinal system to our central nervous system, highlighting the influence of gut health on mental well-being. The microbiome, consisting of trillions of microorganisms residing in our intestines, plays a critical role in this phenomenon. Various studies have indicated that a diverse and balanced microbiome can positively impact mood and emotional health, while dysbiosis, or an imbalance in gut bacteria, may contribute to mental health disorders such as anxiety and depression.
We also discussed how the gut microbiota can affect neurotransmitter production, inflammation levels, and the body’s stress response. For instance, certain beneficial bacteria are known to synthesize neurotransmitters like serotonin, which is often referred to as the “feel-good” chemical. Conversely, an unhealthy microbiome can hinder the production of these essential compounds, potentially leading to mood disturbances. The role of dietary habits cannot be overlooked, as what we consume significantly influences the composition of our gut microbiota.
In essence, recognizing the importance of the gut-brain axis emphasizes the need for a holistic approach to mental health. By focusing on nurturing our microbiome through balanced nutrition, physical activity, and stress management, we can improve not only our digestive health but also our emotional resilience. As research continues to unveil the complexities of this relationship, we anticipate that future findings will pave the way for innovative strategies in mental health treatment, encouraging individuals to consider their gut health as a vital component of their overall wellness. Overall, a healthy microbiome has the potential to lead to improved mood and psychological outcomes, bridging the gap between our gut and mind.