Introduction
The landscape of medical device technologies is continuously evolving, playing a crucial role in the enhancement of healthcare delivery. As innovations emerge, the integration of advanced medical devices is fundamentally transforming patient care, diagnostics, and treatment options. With the rise of technologies such as telemedicine, remote monitoring, and robotic-assisted surgeries, healthcare systems are beginning to adopt more efficient solutions that not only improve operational effectiveness but also significantly enhance patient outcomes. These advancements are not merely adjuncts to existing practices; rather, they represent a paradigm shift in how healthcare is delivered and experienced globally.
At the heart of these innovations lies a commitment to improving patient care. Medical devices are increasingly designed with user-centered results in mind, facilitating better diagnosis and treatment pathways. For example, the introduction of wearable health technology allows patients and healthcare providers to access real-time health data, enabling proactive health management and timely interventions. Similarly, the deployment of artificial intelligence in medical imaging devices enhances the accuracy of diagnostics, leading to better treatment plans and reduced waiting times for patients.
This blog aims to provide insights into the top 10 medical device technologies that are anticipated to shape the future of healthcare. By exploring these innovations, we will highlight their significance within the healthcare ecosystem and their capacity to address current challenges. As the medical device industry continues to innovate, understanding the impact of these technologies is essential for healthcare professionals, policymakers, and patients alike. The chosen technologies for examination in this post showcase the ongoing evolution and transformative potential of medical devices in delivering comprehensive, quality healthcare.
1. Wearable Health Technology
Wearable technology is no longer confined to fitness enthusiasts tracking their daily steps. It has become a vital component in healthcare, allowing real-time monitoring of critical health metrics such as heart rate, oxygen levels, sleep patterns, and more. Wearables have revolutionized chronic disease management, preventive care, and wellness by empowering patients to take control of their health.
Wearable health technology refers to electronic devices designed to be worn on the body, often integrating sensors and software to track various aspects of a person’s health. These devices collect data such as heart rate, physical activity, sleep patterns, and even blood oxygen levels, providing users and healthcare professionals with valuable insights into overall well-being.
Some of the most common types of wearable health devices include:
- Fitness Trackers (e.g., Fitbit, Garmin): Primarily used for tracking steps, calories burned, and exercise routines.
- Smartwatches (e.g., Apple Watch, Samsung Galaxy Watch): These offer more comprehensive health monitoring, including heart rate, ECG readings, and blood oxygen levels.
- Wearable ECG Monitors (e.g., AliveCor Kardia): Medical-grade devices that track heart rhythms and can detect conditions like atrial fibrillation.
- Wearable Blood Pressure Monitors: Devices like Omron’s wearable blood pressure monitors provide continuous blood pressure tracking in a compact, convenient form.
Key Features and Capabilities
Wearable health devices offer a wide range of features, depending on the type and level of sophistication. Here are some of the most common capabilities:
- Activity Tracking
Basic wearables track daily activities such as steps taken, distance traveled, and calories burned. More advanced wearables can differentiate between types of exercise (e.g., running, swimming, cycling) and provide detailed metrics on performance. - Heart Rate Monitoring
Almost all health wearables today come with heart rate monitors that provide continuous or on-demand readings. Some advanced devices also offer heart rate variability (HRV) tracking, an indicator of stress levels and cardiovascular health. - Sleep Monitoring
Many wearables include sleep tracking features that monitor sleep stages (light, deep, and REM sleep) and provide insights into sleep quality and patterns. This helps users understand how much restorative sleep they’re getting and how to improve their sleep hygiene. - Electrocardiogram (ECG) Monitoring
Devices like the Apple Watch and Fitbit Sense can perform an ECG, detecting irregular heart rhythms and potentially identifying serious conditions like atrial fibrillation. This capability brings clinical-level monitoring into the hands of everyday consumers. - Blood Oxygen Monitoring (SpO2)
The ability to monitor blood oxygen levels has gained prominence, especially during the COVID-19 pandemic. Wearables like the Apple Watch and Garmin devices can track SpO2 levels, which is critical for understanding respiratory health and detecting conditions like sleep apnea or respiratory infections. - Continuous Glucose Monitoring (CGM)
For individuals with diabetes, continuous glucose monitoring (CGM) devices are a game-changer. These wearables provide real-time blood glucose levels, allowing users to manage their condition more effectively. Devices like the Dexcom G6 and Abbott’s FreeStyle Libre are leading examples of CGMs in the market. - Stress and Mental Health Tracking
Advanced wearables now offer stress tracking, using heart rate variability (HRV) and other metrics to estimate stress levels throughout the day. Some devices also incorporate mindfulness and guided breathing exercises to help manage stress. - Hydration and Temperature Monitoring
Some devices track hydration levels or offer skin temperature monitoring, which can indicate illness or infection. These features are particularly useful for athletes and individuals looking to optimize their physical performance or detect early signs of health issues.
Applications:
- Chronic Disease Management: Devices such as continuous glucose monitors (CGM) help diabetic patients monitor blood sugar levels in real-time.
- Cardiovascular Health: Wearables like the Apple Watch can detect irregular heart rhythms and alert users about potential arrhythmias, offering early warning for conditions such as atrial fibrillation.
- Fitness and Wellness: Wearables help users track fitness metrics, sleep patterns, and overall physical activity.
Market Insights:
- Global Market Size: The wearable healthcare market was valued at $18.61 billion in 2021 and is expected to grow to $195 billion by 2030.
- Growth Drivers: Increased awareness of health and fitness, a rise in chronic diseases, and the aging population are driving the demand for wearable health technologies.

Future Trends:
The integration of AI and machine learning (ML) into wearables will enhance predictive analytics, enabling wearables to predict potential health risks before they manifest. As wearable devices become more sophisticated, they will play an even more critical role in personalized healthcare, offering tailored recommendations based on individual health data.
2. Artificial Intelligence (AI) and Machine Learning in Diagnostics
Artificial Intelligence (AI) and machine learning (ML) are transforming the way healthcare providers diagnose diseases. AI algorithms can process vast amounts of data, enabling them to detect patterns and correlations that may be missed by human clinicians. AI-powered diagnostics are faster, more accurate, and can help reduce the strain on overworked healthcare professionals.
AI and ML are transforming the field of medical diagnostics by enhancing the accuracy, speed, and efficiency of diagnosing diseases. Here’s a short overview of how they are impacting diagnostics:
1. Improved Diagnostic Accuracy
AI-powered algorithms can analyze large datasets from medical images, lab results, and patient records to detect patterns that might be missed by human eyes. Machine learning models, particularly deep learning, are being used in areas like radiology to detect abnormalities such as tumors in X-rays, CT scans, and MRIs with high accuracy. This reduces human error and enables earlier detection of diseases like cancer.
2. Faster Diagnosis
AI tools can process data in real time, leading to faster diagnostics. For example, AI-driven diagnostic platforms can analyze medical images in seconds, providing quicker feedback to doctors. This is particularly useful in emergency situations or remote areas where specialists may not be readily available.
3. Personalized Medicine
Machine learning algorithms can assess individual patient data to provide personalized diagnostic insights. By analyzing genetic, lifestyle, and environmental data, AI can help predict the likelihood of certain conditions and suggest tailored treatment options, moving toward precision medicine.
4. Integration with Wearables and IoT Devices
AI can be integrated with wearable health technologies, continuously monitoring patients’ vitals and analyzing real-time data. This can lead to the early detection of conditions such as heart disease or diabetes before symptoms become severe, enabling proactive intervention.
5. Reducing Healthcare Costs
By automating parts of the diagnostic process, AI and ML help reduce the time and resources needed for testing, imaging, and analysis, cutting healthcare costs while maintaining high-quality care.
Applications:
- Medical Imaging: AI can analyze CT scans, MRIs, and X-rays to detect abnormalities such as tumors, lesions, or fractures with high accuracy.
- Pathology: AI systems assist pathologists in identifying disease markers in blood samples or tissue biopsies.
- Clinical Decision Support: AI systems help physicians make more informed decisions by providing insights based on patient data and the latest medical research.
Market Insights:
- Global Market Size: The AI in healthcare market was valued at $6.7 billion in 2020 and is projected to grow to $208.2 billion by 2030.
- Growth Drivers: The increasing need for early and accurate diagnosis, advancements in AI technologies, and the growing volume of healthcare data are key drivers.
Future Trends:
AI’s role in healthcare will continue to grow, especially in diagnostics, drug development, and personalized treatment plans. The collaboration between AI and human clinicians will lead to improved diagnostic accuracy and better patient outcomes. Additionally, AI will become integral to virtual health assistants, telemedicine, and remote monitoring, further decentralizing healthcare services.
3. Robotic Surgery and Minimally Invasive Devices
Robotic-assisted surgery is one of the most significant advancements in medical device technology, allowing for precision and control that surpasses traditional surgical methods. Minimally invasive surgeries are becoming the norm, reducing patient recovery times, decreasing the risk of infections, and enhancing surgical outcomes.
Robotic surgery and minimally invasive devices are revolutionizing surgical procedures by offering greater precision, reduced trauma, and faster recovery times for patients.
1. Robotic Surgery
Robotic surgery uses advanced robotic systems controlled by a surgeon to perform complex procedures with enhanced precision. The most common system is the da Vinci Surgical System, which allows for highly controlled and flexible instrument movements beyond human capabilities. Key benefits include:
- Precision: Robotic arms filter out any tremors and allow for highly precise movements, especially in delicate areas.
- Smaller Incisions: Procedures are performed through small incisions, reducing scarring, blood loss, and the risk of infection.
- Better Visualization: 3D high-definition cameras provide detailed views of the surgical site, improving accuracy.
Robotic surgery is commonly used for urologic, gynecologic, and cardiovascular procedures, as well as cancer treatments.
2. Minimally Invasive Devices
Minimally invasive devices are used in procedures that avoid large incisions, reducing the impact on the body. Common techniques include laparoscopy and endoscopy, where small tools and cameras are inserted through tiny cuts or natural openings. Benefits include:
- Faster Recovery: Patients heal more quickly, with less post-operative pain and shorter hospital stays.
- Less Risk: Reduced trauma to tissues and organs, leading to fewer complications.
- Better Outcomes: These techniques are associated with lower rates of infection and better cosmetic results.
Minimally invasive devices are widely used in surgeries like gallbladder removal, hernia repair, and orthopedic procedures.
Applications:
- Orthopedic Surgery: Robotic systems like MAKO are used for joint replacements and other orthopedic surgeries, providing precision and improving recovery outcomes.
- General Surgery: The Da Vinci Surgical System is used for complex procedures such as prostatectomy, hysterectomy, and heart valve repair, offering unparalleled control to surgeons.
- Neurosurgery: Robotics are used in brain surgery to remove tumors or treat neurological disorders with high precision.
Market Insights:
- Global Market Size: The robotic surgery market was valued at $6.1 billion in 2020 and is expected to reach $14.4 billion by 2028.
- Growth Drivers: Rising demand for precision in surgeries, shorter recovery times, and the increasing adoption of robotic systems by hospitals are driving the market.
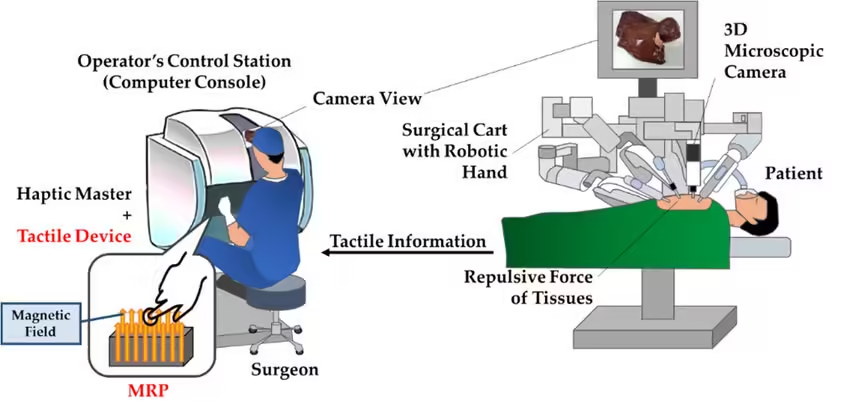
Future Trends:
Robotic surgery systems will continue to evolve, with advancements in haptic feedback, machine learning, and real-time imaging. Surgeons will have even greater control over procedures, allowing for more complex surgeries to be performed robotically. Furthermore, as the cost of these systems decreases, they will become more widely available in hospitals globally.
4. 3D Printing in Medical Devices
3D printing is transforming the medical device industry by enabling the creation of customized implants, prosthetics, and surgical tools tailored to individual patients. This technology allows for rapid prototyping, personalized medicine, and reduced production costs.
3D printing is transforming the medical field by enabling the creation of highly customized and complex medical devices, implants, and anatomical models.
1. Customization
3D printing allows for the production of patient-specific implants and prosthetics tailored to an individual’s unique anatomy. This is particularly useful in areas like orthopedic implants (e.g., hip or knee replacements) and dental restorations, ensuring a perfect fit and improving functionality.
2. Surgical Planning
Doctors use 3D-printed anatomical models based on patient scans to better plan and practice complex surgeries. These models offer a tangible, precise representation of organs, bones, or tumors, enhancing surgical precision and reducing risks.
3. Organ and Tissue Scaffolds
Researchers are using 3D printing to create bioprinted tissue scaffolds, which support the growth of cells to regenerate tissues or potentially even organs. Though still in early stages, this could revolutionize transplants by reducing the need for donor organs.
4. Rapid Prototyping
3D printing allows for the fast and cost-effective development of prototypes for medical devices, enabling quicker innovation and testing of new designs. This accelerates the time it takes for medical innovations to reach the market.
5. Cost Efficiency
3D printing reduces the cost of producing custom medical devices by eliminating the need for traditional manufacturing methods and molds. This helps lower production costs and makes healthcare more accessible.
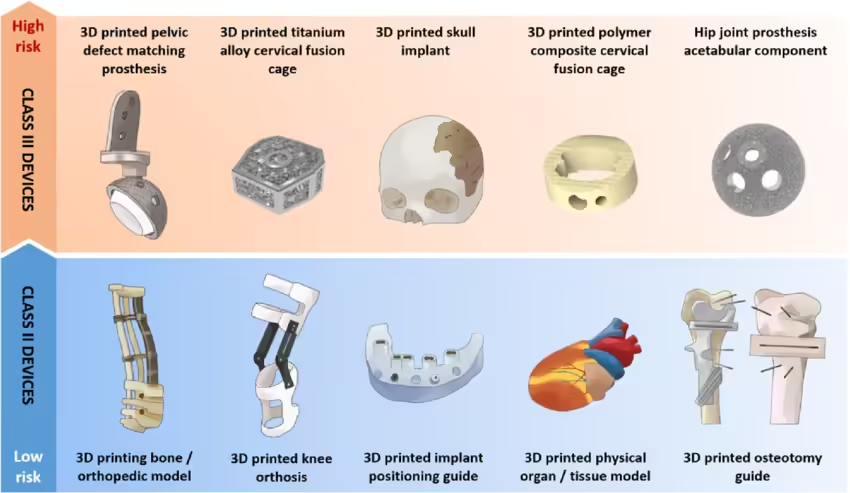
Applications:
- Prosthetics and Orthotics: Custom 3D-printed prosthetics are revolutionizing the lives of amputees by offering devices that perfectly fit their anatomy.
- Surgical Models: Surgeons use 3D-printed models of organs or bones to practice and plan complex procedures.
- Dental Implants: Dentists use 3D printing to create custom dental implants, crowns, and braces.
Market Insights:
- Global Market Size: The 3D printing medical devices market was valued at $2.53 billion in 2020 and is expected to grow to $6.08 billion by 2027.
- Growth Drivers: The rising demand for customized medical devices, advances in 3D printing materials and technologies, and the increasing prevalence of orthopedic and dental conditions.
Future Trends:
Bioprinting, a subfield of 3D printing, is a rapidly growing area. Researchers are developing methods to print human tissues and organs, which could one day solve the organ donor shortage crisis. The technology also holds the potential to produce personalized, patient-specific organs and tissues, significantly improving the outcomes of transplants and surgeries.
5. Telemedicine and Remote Monitoring
Telemedicine has become an essential tool in modern healthcare, especially during the COVID-19 pandemic when access to physical healthcare facilities was limited. Telemedicine allows healthcare providers to offer remote consultations, monitor patients from afar, and manage chronic conditions without requiring in-person visits.
Telemedicine and remote monitoring are transforming healthcare by enabling patients and providers to connect virtually, improving access to care and enhancing chronic disease management.

1. Telemedicine
Telemedicine refers to the use of digital communication technologies (such as video calls, mobile apps, and messaging) to deliver healthcare services remotely. Key benefits include:
- Improved Access to Care: Patients in rural or underserved areas can consult with specialists and receive care without traveling long distances.
- Convenience: Patients can have virtual consultations from the comfort of their homes, saving time and reducing hospital visits.
- Real-time Consultations: Doctors can diagnose, prescribe treatments, and follow up with patients in real time, improving response time for acute conditions.
2. Remote Monitoring
Remote patient monitoring (RPM) involves the use of wearable devices and sensors to track vital signs (such as heart rate, blood pressure, glucose levels) and health conditions continuously. This data is sent to healthcare providers for analysis. Benefits include:
- Chronic Disease Management: Patients with conditions like diabetes, hypertension, or heart disease can be monitored closely, reducing hospital readmissions and improving disease management.
- Proactive Care: Continuous monitoring allows for early detection of health issues, enabling timely intervention before conditions worsen.
- Reduced Healthcare Costs: By minimizing hospital visits and emergencies, RPM helps reduce the overall cost of care.
3. Enhanced Patient Engagement
Telemedicine and remote monitoring empower patients to take an active role in managing their health. Regular data tracking and easy access to healthcare professionals encourage better health outcomes.
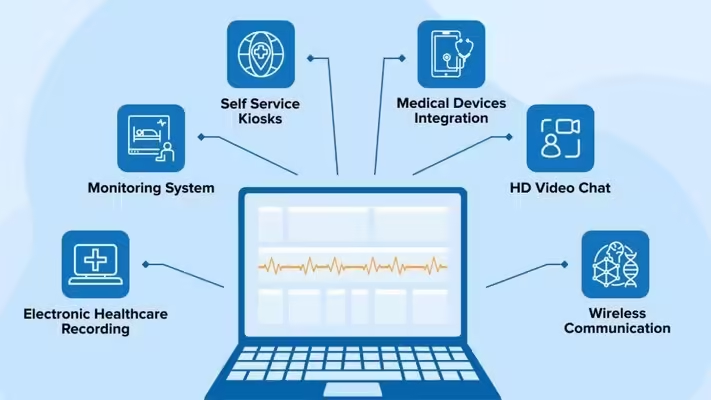
Applications:
- Video Consultations: Patients can connect with doctors through video calls, making healthcare more accessible, particularly in remote areas.
- Remote Patient Monitoring: Devices like blood pressure monitors, glucose monitors, and pulse oximeters send real-time data to healthcare providers.
- Chronic Disease Management: Telemedicine platforms enable continuous monitoring of patients with conditions such as diabetes, hypertension, and heart disease.
Market Insights:
- Global Market Size: The telemedicine market was valued at $55.9 billion in 2020 and is projected to reach $298 billion by 2028.
- Growth Drivers: The increased need for remote healthcare solutions, rising chronic disease prevalence, and advancements in telecommunications infrastructure.
Future Trends:
As broadband access expands globally and 5G becomes more widespread, telemedicine will continue to grow. AI-driven telemedicine platforms will enhance the accuracy of remote consultations, and wearable devices will further streamline remote monitoring. Telemedicine is expected to be integrated into routine healthcare, reducing hospital visits and healthcare costs.
6. Smart Implants
Smart implants are revolutionizing the way medical devices interact with the body. These implants are embedded with sensors that monitor various physiological metrics and transmit data to healthcare providers in real-time. Smart implants enhance patient outcomes by enabling continuous monitoring and timely intervention.
Smart implants are advanced medical devices embedded with sensors or wireless communication technology to provide real-time data and enhanced functionality for patient care.

1. Real-Time Monitoring
Smart implants can continuously monitor vital signs or biological activity and transmit this data to healthcare providers. For example, cardiac pacemakers or neurostimulators send information about heart rhythm or brain activity, allowing doctors to monitor patients remotely and make timely adjustments to treatments.
2. Enhanced Treatment Outcomes
These implants offer personalized treatment by adjusting their performance based on the patient’s needs. Orthopedic smart implants, for instance, can track healing progress after surgery, ensuring the implant is working as expected and aiding in recovery.
3. Drug Delivery Systems
Some smart implants are designed to deliver medications directly to the target area in precise doses. This is particularly useful for patients with chronic conditions, such as cancer or diabetes, as it reduces the need for frequent injections or oral medication.
4. Early Detection of Complications
Smart implants can detect potential issues, like infections, implant failure, or mechanical stress, before they become serious. Early warning systems allow for immediate interventions, reducing complications and improving patient outcomes.
5. Wireless Communication
Many smart implants use wireless technology to communicate with external devices, such as smartphones or tablets, making it easy for patients and doctors to access real-time data and manage health conditions efficiently.
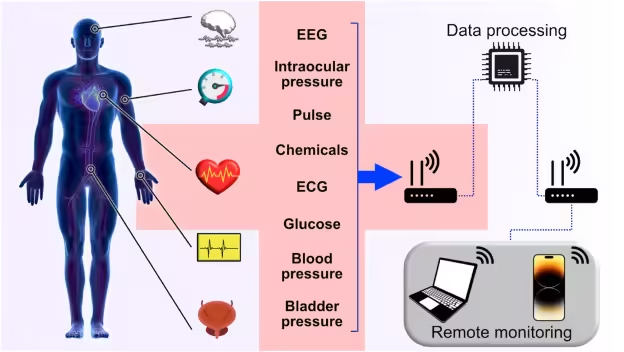
Applications:
- Cardiac Implants: Smart pacemakers and defibrillators can monitor heart rhythms and send data to cardiologists, who can adjust treatments as needed.
- Orthopedic Implants: Smart knee or hip implants track movement and recovery progress, allowing physicians to monitor post-surgery rehabilitation.
- Insulin Pumps: Smart insulin pumps deliver precise amounts of insulin and adjust dosage based on real-time blood glucose levels.
Market Insights:
- Global Market Size: The smart implants market is expected to grow at a CAGR of 10.5% from 2021 to 2028, driven by increasing cases of chronic diseases and the aging population.
- Growth Drivers: The rise in chronic conditions such as diabetes and cardiovascular diseases, coupled with advancements in biomaterials and sensor technologies.
Future Trends:
The integration of AI with smart implants will enable more sophisticated monitoring and predictive analytics, allowing healthcare providers to intervene before conditions worsen. As sensor technology improves, smart implants will become smaller, less invasive, and more widely used in various fields, from orthopedics to neurology.
7. Point-of-Care Diagnostics
Point-of-care diagnostics (POC) have transformed how medical testing is performed, allowing for quick and accurate results at the site of patient care. This technology eliminates the need for centralized laboratory testing, making diagnostics faster and more accessible, particularly in resource-limited settings.
Point-of-care (POC) diagnostics involve medical testing that is performed at or near the site of patient care, providing immediate results without the need for centralized laboratory facilities.
1. Rapid Results
POC diagnostics deliver quick results in real-time, allowing healthcare providers to make immediate decisions. This is crucial in emergency situations, routine checkups, or remote areas where access to lab services is limited.
2. Common POC Tests
Examples include blood glucose meters, pregnancy tests, rapid strep tests, and COVID-19 antigen tests. These tests are simple to perform, often requiring just a small sample like blood, saliva, or urine.
3. Improved Access to Care
By enabling diagnostics in non-hospital settings such as clinics, homes, or rural areas, POC testing makes healthcare more accessible and reduces the need for patients to travel to specialized labs.
4. Enhanced Disease Management
For chronic conditions like diabetes, POC diagnostics allow patients to monitor their health at home. This enables more frequent testing, better disease management, and timely interventions.
5. Cost and Time Efficiency
POC testing eliminates the need for complex lab processes, reducing wait times and healthcare costs, while improving the overall efficiency of diagnosis and treatment.

Applications:
- Blood Glucose Meters: POC devices allow diabetics to measure blood sugar levels instantly, providing immediate feedback on how to manage their condition.
- Rapid Infectious Disease Testing: POC diagnostics are used to quickly diagnose diseases like COVID-19, influenza, and malaria.
- Portable Ultrasound: Handheld ultrasound devices allow for immediate imaging in the field or in remote locations without access to large medical equipment.
Market Insights:
- Global Market Size: The point-of-care diagnostics market was valued at $36.37 billion in 2020 and is projected to grow to $66.5 billion by 2027.
- Growth Drivers: The need for rapid diagnostics in emergency and remote settings, advancements in POC technologies, and the rising prevalence of chronic and infectious diseases.
Future Trends:
The development of miniaturized, portable POC devices will continue to grow, enabling even more rapid and accurate diagnostics in a variety of settings. Furthermore, POC diagnostics will play a crucial role in future pandemics and public health initiatives by providing fast, decentralized testing capabilities.
8. Nanotechnology in Medicine
Nanotechnology is emerging as one of the most promising fields in medical innovation. By working at the molecular level, nanotechnology offers revolutionary applications in drug delivery, diagnostics, and regenerative medicine. It holds the potential to revolutionize how treatments are administered, making them more targeted and effective.
Nanotechnology in medicine involves the use of nanoparticles and nanoscale materials to improve the diagnosis, treatment, and prevention of diseases at a molecular level.
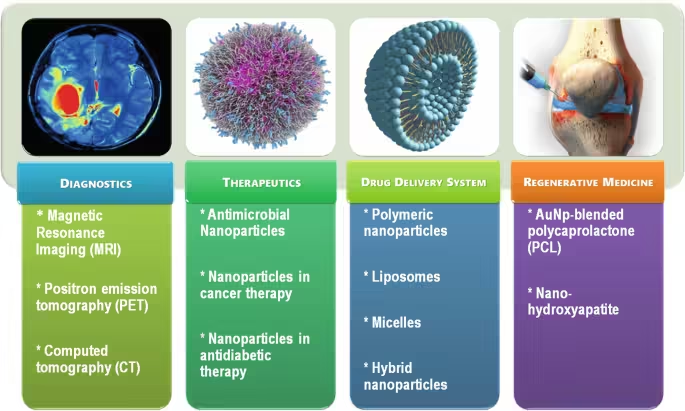
1. Targeted Drug Delivery
Nanoparticles can deliver drugs directly to specific cells or tissues, such as cancer cells, improving the effectiveness of treatments while minimizing side effects on healthy tissues. This targeted approach allows for more precise and efficient therapies, especially in cancer treatment.
2. Improved Diagnostics
Nanotechnology enhances diagnostic techniques through nanosensors and imaging agents that detect diseases earlier and more accurately. For example, nanoparticles can bind to specific biomarkers of diseases, making them easier to detect in blood tests or imaging scans.
3. Regenerative Medicine
Nanotechnology is used to create nanomaterials that help regenerate damaged tissues or organs. Nanoscale scaffolds can support the growth of cells and tissue, promoting healing in conditions like bone fractures or nerve damage.
4. Enhanced Drug Efficacy
Nanoscale drugs can be engineered to improve absorption and effectiveness. Nanomedicine allows drugs to cross biological barriers (e.g., the blood-brain barrier), making treatments for neurological diseases and other hard-to-treat conditions more effective.
5. Minimally Invasive Therapies
Nanotechnology enables minimally invasive treatments, such as using nanorobots or nanoparticles to deliver therapies at the cellular level without the need for major surgery.
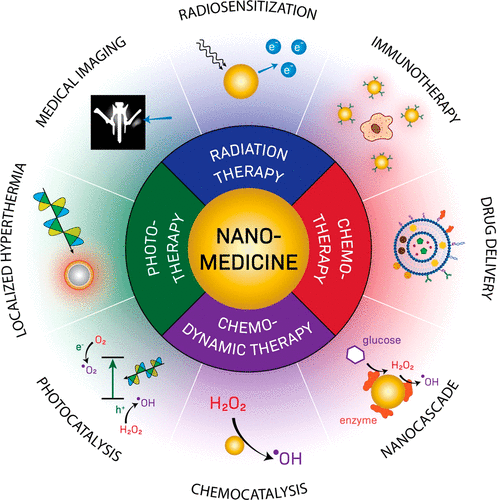
Applications:
- Targeted Drug Delivery: Nanoparticles are used to deliver drugs directly to specific cells or tissues, reducing side effects and improving treatment efficacy, particularly in cancer therapy.
- Nanodiagnostics: Nanotechnology is used in the detection of biomarkers for early disease diagnosis, including cancer and cardiovascular diseases.
- Tissue Engineering: Nanomaterials are being used to develop scaffolds that promote tissue regeneration, offering solutions for organ repair and wound healing.
Market Insights:
- Global Market Size: The global nanotechnology market in medicine was valued at $172.7 billion in 2020 and is projected to reach $393.1 billion by 2030.
- Growth Drivers: Rising demand for precision medicine, advancements in drug delivery systems, and increased focus on chronic disease management.
Future Trends:
The development of nanorobots for precise surgical procedures and the creation of nano-sized biosensors for real-time monitoring of diseases will continue to drive innovation in this field. As research advances, nanotechnology will play an increasingly critical role in personalized medicine, offering treatments tailored to individual patients at the molecular level.
9. Augmented Reality (AR) and Virtual Reality (VR) in Medical Training
Augmented reality (AR) and virtual reality (VR) are revolutionizing medical training and surgery. These technologies provide immersive, hands-on training experiences for medical students and professionals, without putting patients at risk. They are also being used to guide surgeons during complex procedures, enhancing precision and outcomes.
AR and VR are revolutionizing medical education by providing immersive, hands-on learning experiences without the need for real patients.

1. Enhanced Simulation
VR creates fully immersive virtual environments where medical students and professionals can practice complex procedures, such as surgeries, in a risk-free setting. This enhances their skills and confidence before working with actual patients.
2. Augmented Visualization
AR overlays digital information onto the real world, allowing users to see 3D anatomical models and real-time data during procedures. For example, during surgery, AR can project internal structures onto the patient’s body, improving precision.
3. Interactive Learning
Both AR and VR offer interactive learning environments, where users can engage with virtual patients, explore anatomy, and simulate various clinical scenarios. This improves retention of knowledge and practical skills.
4. Remote Training
AR and VR enable remote learning, allowing medical professionals to participate in training sessions or surgeries from anywhere in the world. This expands access to high-quality education and expert guidance.
5. Safe and Cost-Effective
By reducing the need for physical cadavers and real patients, AR and VR provide cost-effective and safe training environments, minimizing risks while ensuring comprehensive education.

Applications:
- Surgical Simulations: VR is used to create realistic surgical simulations, allowing surgeons to practice procedures in a risk-free environment.
- AR in Surgery: AR overlays real-time data and 3D models onto a surgeon’s field of view, helping guide them through complex operations.
- Medical Education: Medical students use VR to study anatomy, practice diagnostic skills, and simulate patient interactions.
Market Insights:
- Global Market Size: The AR/VR in healthcare market was valued at $2.06 billion in 2020 and is projected to grow to $9.82 billion by 2028.
- Growth Drivers: The increasing adoption of AR and VR for medical training, the need for remote learning solutions, and advancements in 3D imaging technologies.
Future Trends:
The use of AR and VR in medical training and surgery will continue to grow, especially as the technology becomes more affordable and accessible. In the future, these technologies may become standard practice in medical schools and operating rooms, offering new ways to visualize complex surgeries and train medical professionals in a controlled, virtual environment.
10. Next-Generation Biometric Devices
Biometric devices are becoming an integral part of healthcare, providing secure, accurate identification of patients and healthcare professionals. These devices use biological data such as fingerprints, iris scans, and facial recognition to verify identities, improve security, and track patient health metrics.
Next-generation biometric devices use advanced technologies to identify individuals based on unique biological traits, offering enhanced security and personalized healthcare applications.
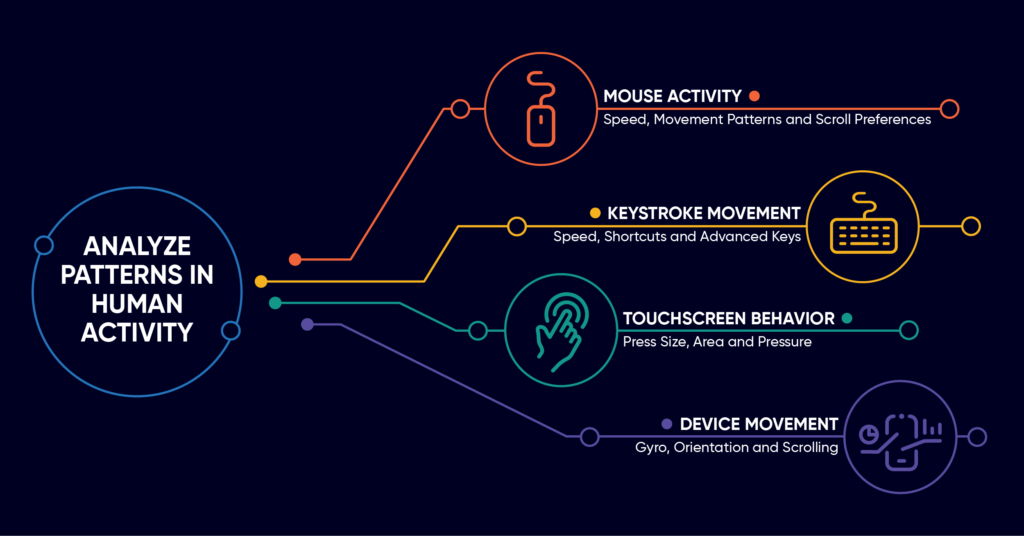
1. Multimodal Biometrics
Next-gen devices combine multiple biometric modalities, such as fingerprint recognition, facial recognition, iris scanning, and voice authentication. This enhances accuracy and security by cross-verifying different identifiers.
2. Continuous Authentication
New biometric devices can enable continuous authentication, where users are verified in real-time as they interact with a system, improving security in sensitive environments like healthcare or financial services.
3. Healthcare Applications
Biometric devices are being used in health monitoring, allowing for non-invasive tracking of vitals such as heart rate or oxygen levels. Devices can also identify patients in hospital settings to ensure personalized treatment and prevent medical errors.
4. Wearable Biometrics
Wearables like smartwatches now include biometric sensors that track health metrics like ECG, blood pressure, and glucose levels, providing real-time data for continuous health monitoring and disease management.
5. Data Security and Privacy
Next-generation biometric devices focus on improving data encryption and privacy protection, ensuring that sensitive biometric data is stored and transmitted securely, addressing privacy concerns in various industries.
Applications:
- Patient Identification: Biometric scanners ensure accurate patient identification, reducing the risk of medical errors and enhancing data security.
- Access Control: Hospitals and healthcare facilities use biometric systems to control access to secure areas, protecting sensitive patient data and medical equipment.
- Health Monitoring: Biometric sensors embedded in wearable devices track physiological data such as heart rate, blood oxygen levels, and temperature.
Market Insights:
- Global Market Size: The biometric devices market in healthcare was valued at $3.25 billion in 2020 and is expected to grow to $68.6 billion by 2027.
- Growth Drivers: Increasing focus on patient data security, rising adoption of wearable biometric devices, and the need for accurate patient identification systems.
Future Trends:
As the healthcare industry moves toward digital transformation, biometric devices will become more widespread. These devices will be integrated into a wide range of medical technologies, offering enhanced security, improved patient identification, and real-time health monitoring. Additionally, biometric devices will play a crucial role in telemedicine, enabling secure remote consultations and patient authentication.
Conclusion
The healthcare industry is experiencing a rapid transformation, driven by technological advancements in medical devices. These top 10 medical device technologies—from AI in diagnostics to nanotechnology and robotic surgeries—are not only improving patient outcomes but also enhancing the efficiency and accessibility of healthcare.
As the demand for personalized care, real-time health monitoring, and minimally invasive procedures increases, these innovations will continue to shape the future of healthcare. The global medical device market is poised for exponential growth, with these technologies leading the charge in creating a more connected, patient-centered, and efficient healthcare ecosystem.
Understanding the current market insights and trends surrounding these technologies will help healthcare providers, investors, and policymakers stay ahead of the curve, ensuring that they are well-prepared for the future of healthcare. These technologies are not just the future; they are already making a significant impact today, paving the way for a healthier and more technologically advanced world.